Obesity and COVID-19: Policy statement
World Obesity Federation commends the World Health Organization (WHO) and most governments around the world for their leadership and rapid and comprehensive action to control this pandemic. The past few months have given us an opportunity to reflect on the wider impacts of COVID-19 on obesity and non-communicable diseases (NCDs), both in the short- and long-term.
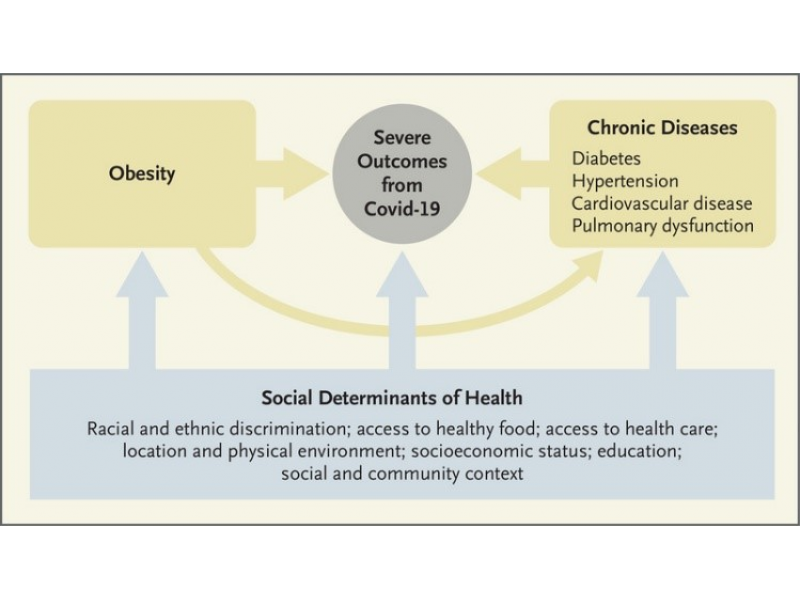
The WHO has highlighted NCDs as a risk factor for becoming seriously ill with COVID-19 [1]. Today, the emerging evidence based on experience from other viral infections and new studies suggest that overweight and obesity seem to be risk factors for worse outcomes in those who are infected by COVID-19. Systematic reviews and meta-analyses overwhelmingly show that obesity is associated both with a higher risk for intensive care unit (ICU) admission and poorer outcomes for COVID-19 [2-4]. In the UK, a report flags that out of 10,465 patients critically ill with confirmed COVID-19, 73.7% were living with overweight or obesity [5]. Meanwhile, a report from Italy suggests 99% of deaths have been in patients with pre-existing conditions, including those which are commonly seen in people with obesity such as hypertension, cancer, diabetes and heart diseases. [6] Overweight and obesity also seem to be risk factors for worse outcomes in younger populations (<60 years old), with patients with a body mass index (BMI) between 30 and 34 being twice as likely to be admitted to ICU compared to individuals with a BMI under 30 [7].
The COVID-19 pandemic and the measures that have had to be taken to help curb COVID-19 are likely to have a number of impacts for people living with obesity, as well as on the health of the general population. The pandemic has shed light on existing challenges including a lack of health coverage and access to adequate care, infrastructure challenges both within and outside the health system, and the perpetuation of weight stigma [8].
A number of these also represent underlying root causes of obesity and thus risk exacerbating the risk of obesity. The first phase of the pandemic showed:
- Strained food systems and supply chains due to concerns of food shortages, as well as an increased reliance on processed, long-life foods and a reduction in fresh fruit and vegetables and unprocessed meat.
- Changes in eating behaviours due to lockdowns, especially for children. A survey conducted in Verona, Italy revealed that 44.5% of respondents increased consumption of sweets, and 44% of respondents mentioned weight gain due to higher calorie intake related and lower levels of physical activity [9]. The survey revealed a significant increase in the consumption of foods high in fat, sugar and salt (HFSS) and an increase in sedentary behaviours, with children spending an additional five hours per day in front of a computer, phone or TV screen.
- Food insecurity amongst the most vulnerable who have reduced access to shops and may have reduced access to normal food assistance programmes e.g. due to school closures. Access to a healthy and sustainable diet is a direct consequence of the “conditions and environment in which one lives.” [10] Today, unhealthy diets are the leading underlying cause of death. Nutritional disparities are driven by socioeconomic, educational and environmental factors. Among all five New York’s boroughs, the Bronx – a borough with high rates of obesity due to poverty and food insecurity – reports the highest hospitalisations and death rates from COVID-19 (Figure 1).



- Reduced opportunities for people to be physically active as movement is restricted. A study using data from a UK-wide online survey highlighted that out of 5,800 adults aged 20 and over, a quarter of them adopted lower intensity physical activity, and included a greater proportion of adults with underlying health conditions [11].
- An impact on mental health, due the seriousness of the emerging situation and challenges faced from isolation, reduced physical activity, social engagement and employment changes.
- Rise in the exposure to opportunistic marketing and distribution of unhealthy commodities and HFSS products. Evidence suggests that the marketing of HFSS products is directly linked to an increase in overweight and obesity in children. However, today 70% of countries still fail to have policies in place to restrict food marketing to children. Furthermore, a report in Brazil shed light on industries’ opportunistic behaviour on the basis of social and philanthropic responsibility [12]. This included the distribution of products such as chocolate milk, cookies, processed meats and so on to health professionals and other essential workers.
- Impacts on health systems and exacerbated challenges for treatment access for people living with obesity, including potential reductions in elective surgical procedures (e.g. bariatric surgery), and modifications to or curtailment of multidisciplinary team management, group weight loss programs and other forms of ambulatory care.

COVID-19 has exposed vulnerabilities in the current food system, our surrounding environments and the absence of processes to protect the health of vulnerable populations. We therefore urge governments around the world to embed the following considerations in their strategies for monitoring and reducing COVID-19 in the short- and long-term to ensure that the wider health of populations is maintained, and the negative impact minimised at this challenging time:
- Ensure that nutritionally adequate food is made available for all, particularly for vulnerable populations such as those with existing health conditions, the elderly, people with disabilities and low-income households
- Ensure that nutrition responses integrate and address malnutrition in all its forms, including overweight and obesity
- Address the upstream factors influencing obesity including lack of access to healthy food, poor diets, food insecurity, built environments, social context, access to health services and education
- Ensure that any policies and restrictions that are put in place to limit the spread of COVID also allow for people to be physically active in open spaces, while still maintaining adequate social distancing. These should include “strategies to facilitate health promoting levels of physical activity in vulnerable groups, including those with both objective and subjective risks.”
- Provide information to the population through the media and social media which provides clear and transparent guidance, dispels myths and promotes mental and physical health during periods of isolation
- Recognise the risk that the present situation has on mental health, and promote strategies to improve and manage this during this challenging time
- Provide helplines and other virtual support services as appropriate for people with existing diseases to ensure they have access to the most up to date information on their care as well as access to the medications required to manage their disease
- Recognise that obesity, and other NCDs appear to increase risk and likely worsen the outcomes of COVID-19 and as such ensure that those people living with these diseases are provided advice if they have symptoms, and where possible tested and provided care early.
For further information with regards to the link between Obesity/NCDs and the current outbreak of COVID-19, explore World Obesity’s policy dossier. We are collating known evidence, resources and materials pertaining to Obesity/NCDs and the current outbreak of COVID-19. We aim to provide an overview of the latest available information regarding any new associations between COVID-19 and obesity and its comorbidities.
- [1] https://www.who.int/internal-publications-detail/covid-19-and-ncds
- [2] https://onlinelibrary.wiley.com/doi/epdf/10.1111/obr.13095
- [3] https://link.springer.com/content/pdf/10.1007/s11356-020-10132-4.pdf
- [4] https://onlinelibrary.wiley.com/doi/epdf/10.1002/jmv.26237
- [5]https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
- [6] https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf
- [7] https://www.medrxiv.org/content/10.1101/2020.05.11.20098806v1.full.pdf
- [8] https://ncdalliance.org/news-events/blog/addressing-obesity-as-part-of-covid-19-responses-vital-for-%E2%80%98building-back-better%E2%80%99
- [9] https://www.crea.gov.it/-/cibo-stili-di-vita-e-bambini-al-tempo-del-covid19-che-cosa-%C3%A8-cambiato-
- [10] https://www.nejm.org/doi/full/10.1056/NEJMp2021264
- [11] https://www.medrxiv.org/content/10.1101/2020.05.12.20098921v1
- [12] https://actbr.org.br/uploads/arquivos/BOLETIM-MONITORAMENTO-JUNHO-EN.pdf
Obesity and COVID-19 policy statement
Obesity and COVID-19 policy statement
Statement from the policy team of World Obesity in regards to the outbreak of Coronavirus (COVID-19) and the implications on those living with obesity, updated August 2020.
Download (252.04 KB)