Global Obesity Forum 2021
On Monday, 20th September, World Obesity convened the Global Obesity Forum. The Forum meets annually to bring together stakeholders representing different parts of the obesity community from across the globe.
This year, the Forum was hosted by the founding members of the Global Obesity Coalition: World Obesity, the World Health Organization (WHO) and UNICEF. For the first time, the event operated a hybrid model, with the 150 invited delegates participating both in New York and online.
Successfully addressing obesity means understanding the “both and” nature of solutions. The ROOTS framework shows that many elements working together - systems, treatment, prevention - are essential. It also means working together and shifting from a narrative in which silos dominate, to one in which there is recognition of the breadth and richness of the needed response, leaving behind false trade-offs; for example, between treatment and prevention, global and national action, and high-, middle- and low-income countries and populations.
Within the context of existing frameworks and commitments, and working with affected populations, WHO, UNICEF and World Obesity founded the Global Obesity Coalition to streamline priority global obesity initiatives and support health and other systems affecting obesity to build back better and more equitably from the COVID-19 pandemic, including incorporating the needs of people with obesity.
The Coalition is organised along three priority areas: shifting the obesity narrative, accelerating implementation of effective actions that promote healthy diets and physical activity, and integrating obesity prevention, management, and treatment into primary health care. These pillars shaped the Forum’s programme, which involved a mix of keynotes, interactive panels and roundtable discussions.



_600_600_s_c1.png)
The event opened with remarks from the three founding organisations. WHO’s Dr Francesco Branca outlined the opportunities to coordinate global strategies across food and health systems, including through the next WHO Executive Board that will look at recommendations on obesity across the life course. Johanna Ralston, CEO of World Obesity, introduced the theme of the day: Changing the narrative. Dispelling myths about obesity as a matter of individual blame rather than societal responsibility is a common objective, and with the Forum happening just days before the UN Food Systems Summit, this message was particularly salient. UNICEF’s Dr Victor Aguayo outlined the objectives of the Coalition, which include facilitating change from a narrative that portrays obesity as a problem for wealthy countries to one that acknowledges the high burden to low- and middle-income countries. The Coalition will also work to accelerate implementation of policies and programmes on affordable diets and discourage the consumption of unhealthy foods, including stopping the marketing of unhealthy foods to children and young people.
Food systems were a hot topic during the Forum, explored in the first panel moderated by Alexey Kotov (Vital Strategies) that featured Prof K. Srinath Reddy (Public Health Foundation of India), Gerda Verburg (SUN Movement) and Lorena Allemandi (NCD Alliance). The speakers debated the tensions between the ‘what’ and the ‘how’ of addressing obesity in food systems and were challenged to share ideas on the priorities for action.

Lorena Allemandi highlighted the need for a strong civil society to break down barriers to progress and help to move the dial. Gerda Verburg responded that it is not enough to know what to do: “The ‘what’ is only important if you know the ‘how’, and the ‘how’ must be done in a way that is understood at the country level.” Key to the ‘how’ is a better understanding of political economy, e.g., how to make nutrition a re-election issue for politicians: “We must work out how to influence decision-makers, through making the political business case”. Prof K. Reddy emphasised that different forms of malnutrition cannot be compartmentalised either separately or sequentially – they are all part of an overlapping scenario, which is all too clear in India where there is a growing ‘triple burden of malnutrition’. This is not about individual responsibility: “We need greater health literacy, but we also need to fix the food system that is promoting unhealthy diets and is responsible for different forms of malnutrition.”

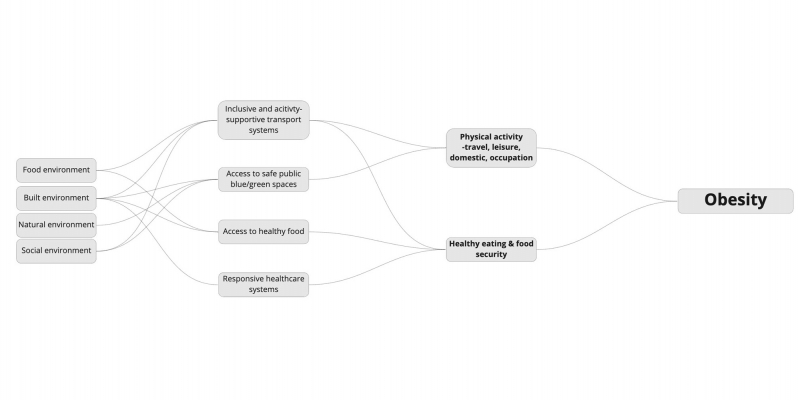
Building on the food system discussions, a keynote presentation by Dr Tolu Oni from Cambridge University explored the systems-based approaches needed to create healthy environments. Dr Oni offered five considerations for taking a systems approach to obesity: equity, entry points, time and space dimensions, future-proofing, and integrated governance. She presented the obesity ecosystem (below), arguing that when focusing on obesity, we often start with the factors that influence individuals, e.g., food and physical activity, but the reality is that we need to go further back upstream. To address obesity, we need to take action across food environments, built environments, natural environments and social environments.
Speaking from Australia, Professor Louise Baur focused her keynote on addressing obesity through health systems. Prof Baur referenced World Obesity research with health professionals from 68 countries on their health systems’ readiness to provide obesity treatment, which found that most do not classify obesity as a disease, that there is an absence of services and lack of trained support, and that stigma is experienced. The Global Obesity Coalition has highlighted the important role of primary health care (PHC) in addressing obesity, especially in low-and middle-income countries. PHC looks at the individual, family and immediate community, and, for example, obesity prevention can be integrated into early childhood care through appropriate complementary feeding and limiting screen time. Prof Baur also raised the need to ‘decolonise obesity’ and for health-system interventions developed in high income countries to be contextualised. Investment in health worker training will be essential, as will addressing weight bias in health systems.
Participants then moved into breakout rooms to deep dive on the Coalition pillars and come up with priorities for action. The breakouts were conducted under Chatham House rules, but an outline of the topics discussed is shared below.
The flawed framing of obesity has led to stigmatisation and discrimination against people living with obesity, siloed approaches to prevention and treatment, and political inaction across the board. Changing the narrative is further complicated by the many norms and realities surrounding obesity. In developed countries, the prevailing myth is that obesity is a personal failure; in other societies, obesity may be associated with affluence and good health.
Furthermore, as Prof Reddy described, a ‘triple burden’ of malnutrition – undernutrition and micronutrient deficiencies combined with obesity and diet-related noncommunicable diseases – is prevalent in many parts of the world, complicating the policy response, often against a background of scarce resources. This discussion identified promising ways to change the narrative and looked at ways to ensure that narrative(s) are inclusive, particularly of people living with obesity: “We must give space to people to show their own lived experience of their obesity and to close the gap between vision and mission.”
We live in environments characterised by low availability, accessibility, and affordability of healthy foods and aggressive marketing of unhealthy foods, including snacks and sugary beverages. At the same time, many of our physical environments are not conducive to people being active as part of everyday life – for example, urban design that encourages motorised traffic and insufficient green and safe space for exercise and active recreation.
As the Forum took place ahead of two important global food events - the UN Food Systems Summit (23 September) and the Nutrition for Growth conference (December) – the discussion concentrated on dietary and food system interventions. In conclusion, the group had three wishes: 1) that the food industry should not be at the policymaking table; 2) that governments are accountable for implementing policies they commit to; 3) that future generations should be prioritised by working with young people.
Even before COVID-19 disrupted primary health services and obesity care worldwide, there were serious shortfalls in the provision of obesity services. There is an urgent need for more training of primary health care workers in obesity prevention and treatment. Not all countries have professional guidelines for obesity treatment, which need to be appropriately adapted to national contexts. A universal health coverage system whose PHC benefit package encompasses obesity can be an accessible route to the inclusion of obesity within health systems in low- and middle-income countries. As Prof Baur highlighted, PHC can address both obesity prevention – through interventions such as cost-effective counselling around healthy diets and physical activity across the life course – as well as basic treatment and management of obesity.
This is of particular relevance in many low- and middle-income countries, where effective care such as bariatric surgery and pharmacotherapy are not likely to be feasible in the near term, for a majority of the population. Most importantly, integration of obesity into primary care assures earlier acknowledgment and a more rapid pathway to treatment, given that the current approach is one in which individuals often delay seeking services until a co-morbidity such as diabetes or CVD is present.
Drs Fatima Cody Stanford and Saifullah Yusop spoke to the specific challenges and options for earlier intervention in health systems and among underserved populations in the US and Malaysia, and Dr Yusop also emphasised the roles stigma had played in his own journey as a patient. Mario Breiro from UNICEF reinforced the intersection of healthy diets and health systems to address obesity in Mexico.
Many of the actions and policies that can successfully address obesity are well known – but there is also a need for innovation across in research, policy and implementation. This breakout session highlighted some novel approaches to address obesity from different angles – among them, new modelling of the cost of obesity, ‘triple-duty’ actions on obesity as recommended by The Global Syndemic report and innovation in cities (which are where the majority of the world’s population now live).
Discussion on the barriers to and enablers of innovation across obesity research, policy and action helped provide direction on the opportunities and future priorities for the Global Obesity Coalition. Successfully seizing the opportunities presented by COVID-19 will require a shift towards streamlined and purposeful collaboration, cooperation and coordination between different stakeholders, at global and national levels.
The Forum ended in plenary with closing remarks from Prof John Wilding, World Obesity’s President and Vilma Tyler from UNICEF: “This is just the beginning of our work…it is important to continue collaboration, including strengthening partnerships and alliances.”
Download our GOF 2021 speakers
Global Obesity Forum 2021 Speakers
Biographies for all attending speakers and panellists for GOF2021.
Download (11.69 MB)