Disparities in paediatric weight management
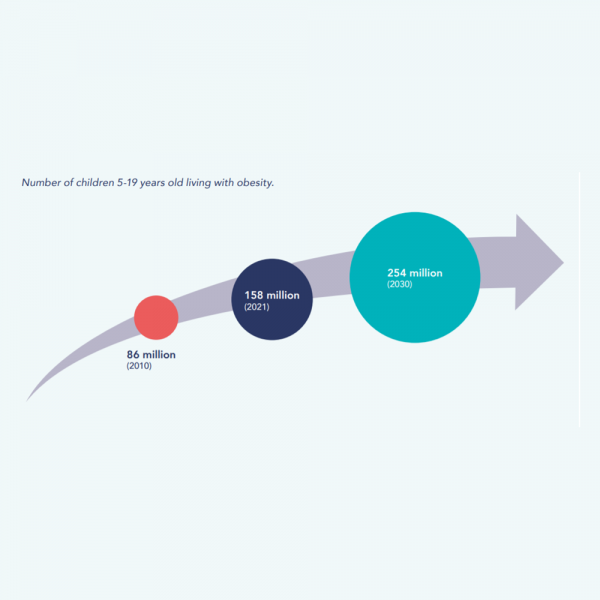
Globally, the rates of childhood obesity are on the rise: by 2020, nearly 160 million children and adolescents were living with obesity, a number predicted to increase to 254 million by 2030.
In developed economies, socially disadvantage children are at greater risk of developing obesity, while in lower- income economies, children from middle and higher-income population groups tend to have higher risks of overweight or obesity.
Socio-economic status and ethnic background are recognised as predictors of risk for the development of obesity in childhood. It follows that paediatric treatment effectiveness may be affected by social disparities. Access to treatment and availability of a range of treatment options may also not be equitably distributed, with absent services and cost barriers adding to disparities in health outcomes. When services are available, treatment may be affected by prevailing assumptions and biases among health care professionals discriminating against some families more than others.
It is therefore essential that interventions are culturally and socially sensitive, avoid stigma, encourage motivation, recognise barriers and reinforce opportunities, while also being achievable within the family’s time and financial resources.
Our new policy brief aims to outline some of the barriers and provide some case studies where service provision attempts to overcome social disparities for children needing care.
While limited, existing evidence allowed us to identify a number of social disparity challenges:
- Families’ perceptions and attitudes to overweight in children
- The role of external environments
- Attrition from treatment
- Treatments costs
- Definitions of obesity

However, around the world, examples are emerging highlighting success, challenges and good practices in paediatric weight management. Based on evidence available in our policy dossier, we formulated the following recommendations for policy makers and health care professionals to improve equitable access to paediatric weight management services:
- Ensure equitable access to treatment
- Increase capacity to ensure services are child-friendly and staff are well trained
- Involve families
- Design interventions in consultation with families and young people, ensuring the recommended treatments are culturally and socially sensitive, avoid stigma, encourage motivation and recognise potential challenges
- Use whole-of-systems approaches incorporating physical activity, diet and psychological components
- Prevent weight re-gain
- Institute political leadership to ensure comprehensive policies and investments to prevent and treat overweight as part of universal health coverage
Download our new policy brief.
Disparities in paediatric weight management
Policy brief analysing case studies and disparities in the treatment of Childhood Obesity, inclusive of recommendations for policy makers and health care professionals.
Download (3.51 MB)